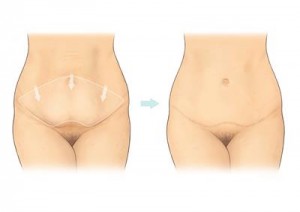
What is an Abdominoplasty?
Abdominoplasty is also known as a ‘tummy tuck’ or as an ‘abdominal resection’. An abdominoplasty is a major operation designed too rejuvenate the abdominal area and remove excess fat and skin. It is often performed for patients who have either lost a lot of weight or to remove the excess loose tissue following child birth. In most cases it restores weakened or separated muscles creating an improved abdominal contour. It is necessary to reposition your umbilicus (tummy button). An abdominoplasty operation will leave a scar from hip to hip and around your umbilicus. It is an operation that is performed under a general anaesthetic. Please visit the BAPRAS link here for further information:
Why am I having an Abdominoplasty?
- An abdominoplasty reduces excess skin from your abdomen following major weight loss
- After successful treatment for obesity or following pregnancy.
- It may also help to tighten abdominal muscles, which have become weakened over a period of time.
What are the alternatives?
There are no alternative treatments which the surgeons can offer you.
Who is unsuitable for a tummy tuck?
Those who have been encouraged to improve their body contour by others. Abdominoplasty surgery is not recommended to people with unrealistic expectations, smokers and those with a significant medical history i.e. diabetes, cardiovascular disease, immunosuppressed. If you plan to have more children, you should consider having them prior to surgery.
What are the risks associated with an Abdominoplasty?
In the majority of cases this operation is carried out very successfully with good cosmetic results. However, as with any operation, there is a chance of side effects or complications. Below is a list of complications that can occur following an abdominoplasty. This list of complications is not intended to put you off having the operation but you need to be aware of any potential complications before you consent to having surgery.
- Bleeding
During or soon after the operation you may experience bleeding from your wound, which can result in a collection of blood (called a haematoma) beneath the wound site. Should this occur you could experience excessive pain and swelling in your abdomen. Healthcare staff will assess this and will offer you painkillers to alleviate this. The collected blood may need to be removed in the operating theatre; this may mean having a further small procedure. Two drains will be required to help minimise the excess blood and fluid in the early post-operative period. These will be removed by a District Nurse or myself at your follow up.
- Loss of skin from your abdomen
During the operation cuts are made through the skin and fat of your abdomen. This tissue always requires a very good blood supply. Sometimes the blood supply to the skin is disrupted and becomes inadequate. This means some of your skin may not be viable causing another wound on the surface of your abdomen; (This is called skin necrosis). Should this happen, healing to your wound will be delayed and extra scarring may occur. A further implication of skin loss may be the need for further surgery to correct the problem. This may include vacuum dressings or a skin graft operation at a later date.
- Fat necrosis
Your abdomen contains large amounts of fatty tissue beneath the skin which can have a reduced blood supply after the operation and cause long term lumpiness and distortion.
- Chest infection
A chest infection can occur following any general anaesthetic. You can help to reduce the risk of this happening by taking regular deep breaths following surgery and getting up and sitting out of bed as soon as you are well enough. If you smoke or vape you can reduce the risk of a chest infection by stopping for at least six weeks prior to your operation.
- Anaesthetic risks and complications
Your operation will be carried under a general anaesthetic. Your anaesthetist will give you more information about your anaesthetic and will discuss anaesthetic risks and complications with you prior to your surgery following an assessment.
- Umbilical necrosis
During the operation your umbilicus (belly button) will need to be repositioned. There is a small risk that by repositioning the belly button all or part of the skin of your belly button to die. If this happens healing will be delayed and you may need another operation to correct the problem.
- Fluid collection beneath the wound
There is a risk that fluid may pool beneath your stitch line after surgery (this is called a seroma). A seroma can occur at any time after the operation. This fluid is usually re-absorbed by the body over a period of time. There are situations in which a doctor may need to remove the fluid using a small needle and syringe if the seroma causes pain and discomfort. In some cases the fluid can collect again so this procedure may need to be done more than once. This happens on occasions to other patients and the surgeon will discuss the risks of a seroma with you before your operation. As mentioned before two drains will be inserted to minimise seroma collection.
- Wound infection
A wound infection can occur at any time following surgery. If your wound becomes infected you may need treatment with antibiotics or you may require hospital admission for further surgery to drain and treat the infection. Signs and symptoms of wound infection can include increased swelling, redness, fluid leakage and increased pain in your abdomen.
- Wound breakdown
Wound breakdown can occur following surgery. Often there is some delay in healing of the stitch line. However; in rare cases the stitch line may not heal properly and the wound may breakdown or gape open. As a result, dressings will be required for prolonged periods and a further operation maybe needed to hasten healing and/or minimise the distortion that this complication can sometimes cause. If you smoke or vape you can reduce the risk of a chest infection by stopping for at least three months prior to your operation.
- Excess or abnormal scarring
You will have a permanent, scar on your skin. Your scar can be concealed by clothing, however this cannot be guaranteed by the types of clothing you decide to wear. Your scar can sometimes improve over a period of 18 months following surgery however; some people for unknown reasons, develop raised, red and lumpy scars. Unfortunately this is largely beyond the control of the surgeon. The chances of this occurring are greater if you have already developed thickened scars following accidents or operations elsewhere. Scars sometimes stretch as they mature and this is also largely beyond surgical control.
- Fat necrosis
During your operation cuts will be made through fat tissue. Rarely the blood supply to this area becomes disrupted, causing this tissue to become non viable. Should this happen the fatty tissue can become liquified and start to leak out of the wound (fat necrosis). This may mean having another operation to correct the cause and correct any deformities.
- Asymmetry of the umbilicus and scarring
During an abdominoplasty operation your surgeon will need to reposition your umbilicus (belly button). There is a risk that your umbilicus may not be placed centrally on your abdomen (as it was before your operation). Some degree of asymmetry of your scar may also be evident. If you are concerned about asymmetry after your scars have had at least 12 months to settle you should discuss this with your surgeon.
- Dog-ears
Once your wounds are healed you may notice an excess of skin at either end of the stitch line, these are known as dog-ears. If these have not settled down after 12 months, it is best to discuss further management with your surgeon. A further operation may be necessary to correct this.
- Altered sensation in your thigh and abdominal skin
You may experience some numbness in the lower part of your abdomen and thighs after this operation. In the majority of people this numbness reduces over a period of 12 months following surgery. Sometimes a small number of people may experience permanent numbness of their skin following abdominoplasty.
- Deep vein thrombosis (DVT)
This is a blood clot that arises in the deep veins of the leg or pelvis. A deep vein thrombosis can happen if your mobility is restricted or you are inactive for a time following your operation. You may be given injections that help to prevent this from happening. You can reduce the risk of deep vein thrombosis by wearing the elastic stockings supplied during and after your operation and moving your legs about whilst you are in bed. Getting up and walking as soon as you are well enough may also reduce the risk of a DVT.
- Pulmonary Embolism (PE)
This is a portion of blood clot that has become lodged in a small blood vessel in your lung. It can cut off some of the blood supply to your lung causing shortness of breath or pain when you breathe in deeply. PE is a serious complication of surgery. You can reduce the risk of PE by following the advice for the prevention of DVT listed above. Patients are offered injections which help thin the blood after their operation as mobility may be limited and this can sometimes predispose to a PE or DVT. If you take the oral contraceptive pill or HRT you may be contacted by the hospital and asked to stop taking them. If you do stop taking the contraceptive pill remember to use some other method of contraception to avoid pregnancy. If you do not hear from the hospital, then continue to take your medication as normal. You will be asked to attend a pre assessment clinic at Frimley Park Hospital. These investigations will include a blood test. Photographs may be taken of your abdomen for your medical records and you will be asked for permission for the photographs to be taken.
There may be other risks specific to your individual case. The surgeon or ward nurse will discuss any further risks with you.
How do I prepare for my operation?
Please be prepared to take up to four weeks off work to recuperate depending on your type of work.
If you are overweight you will be asked to reduce your weight to within normal limits for your height. You will need to achieve this weight reduction before admission to hospital. If you need help to reach your target weight your GP may be able to refer you to a dietician.
If your GP prescribes aspirin, ibuprofen or other medications which may cause bruising or bleeding such as clopidogrel or Vioxx, you may be asked to stop taking these for a period of seven days before your operation. These medications may increase the risk of bleeding during and after your operation. Your surgeon will advise you about this when you see him / her in clinic. If you do not hear from the hospital, then continue to take your medication as normal.
If you normally take warfarin tablets you may be asked to stop taking these 5 days before your operation. You may also be asked to have a blood test on the day of your operation.
What happens when I come into hospital?
A doctor will make sure that you are informed about the nature of your surgery and the possible complications. He or she will ask you to sign a consent form agreeing to the surgery. On the day of your operation you will need to stop eating and drinking for a period of time, the nursing staff will advise you of when this will be. Please have a bath or shower before your operation. If you have any questions or concerns about your operation please ask a member of the nursing staff for assistance.
What happens after the operation?
The operation will take about 1-2 hours to complete however; you will be in the operating department for longer than this to allow time for recovery. When you wake up from your operation you will be lying in a ‘jack-knifed’ position; this means that you will have pillows under your knees, keeping your hips and knees bent to reduce the tension on your abdomen. You will be asked to sleep with your hips and knees in this position for several days following your operation to reduce the strain on your stitches.
You should not lie on your sides or stomach as this will cause discomfort and will put pressure on your stitches.
Because of the increased risk of thromboembolism you will require calf compression devices, in addition, you will be injected daily with an anticoagulant under the skin which you will need to continue yourself for two weeks after surgery.
The nurse looking after you will regularly check your wound, your drains, your blood pressure and pulse after you return from theatre. You will not have a catheter in place. You will be able to eat, drink and mobilise as soon as the anaesthetic subsides.
There will be bruising, swelling and discomfort following your operation and you will be offered pain relief either by injections, tablets or a patient controlled pain relief pump.
You may have a drip, usually in your hand or arm, to replace any fluid lost during your operation. You may lose blood during your operation; sometimes you may need a blood transfusion to replace this. Alternatively, you may be prescribed iron tablets to correct any associated problems.
You will also have a dressing over your wound.
There will usually be a drain (tube) at either side of your abdomen, which drains away any excess blood into a bottle attached to the drain. These drains will be removed when there is only a small amount of drainage. This can take several days. Your dressing will normally be left in place for up to 10 days unless it becomes wet, in which case it may be changed earlier.
You are encouraged to get up on the day after your operation to help prevent the formation of any blood clots in your legs. You will be asked to walk in a ‘stooped’ position or with your back bent over for a few days to reduce the strain on your stitches.
How long will you stay in hospital?
Normally you can expect to be in hospital for 3-5 days after your operation; however this depends on when your drains are removed and the preferences of your surgeon.
What happens when I go home?
You are normally prescribed a weeks supply of painkillers to take home. If you need a further supply you should contact your own doctor. (GP)
When you are discharged from hospital you should keep fairly mobile but avoid any movements that cause straining or stretching to your abdominal muscles and wound.
You should arrange for a friend or family member to collect you when discharged and have some support at home for the next week. You do not need any special care at home, however if you have small children it may be advisable to arrange for someone to help you to care for them. Please do not use a hot water bottle to relieve abdominal discomfort at any time after your operation, as there is a chance this can damage your skin, as you may be numb in this area and be unaware of excessive heat. You can potentially leak very hot water onto your wound.
Follow up
Whilst in hospital you will be reviewed daily and will be discharged with your drains in place. The ward will arrange for District Nurse to visit you at home and measure your drain output daily. Your dressings will be changed after 7-10 days in clinic. Any staples or stitches will be removed in clinic, usually within two weeks of your operation.
You will have dissolving stitches that do not need to be removed. You will require dressings until your wounds have healed. Once your wounds have healed you should massage your scar regularly with a bland oily based cream such as bio oil or silicone gel/tape as this may help it to settle down and relieve itching. You will be sent an appointment to see your consultant in the out patients department at approximately 1-2 weeks following surgery.
What else can go wrong?
It is normal to have some bruising, swelling and tenderness around your abdomen for several weeks following the operation. However if you suffer from any of the following symptoms after your discharge from hospital you should telephone the numbers provided on your discharge summary for advice:
- Persistent or increasing levels of pain;
- Fever and increase in temperature
- A feeling of heat in your abdomen;
- Redness or swelling of your abdomen;
- Tiredness or fatigue that lasts longer than three weeks.
- Shortness of breath or pain when you breathe in deeply.
When can I resume normal activities again?
You should not drive until you can wear a seat belt comfortably and feel able to perform an emergency stop; this could be up to 6 weeks following surgery. Your insurance company may refuse to meet a claim if they feel you have driven too soon. It is also advisable to contact your insurance company with regards to cover following a general anaesthetic. You should not go back to work until instructed by your surgeon. This could be 4-6 weeks depending on your job. You will be given details on when you can resume activities. Please ask if you need a doctor’s certificate for your work, should you need follow up certificates you should see your GP. You may resume sporting activities approximately 6 weeks after your surgery; however you should stop if you experience pain or discomfort during the activity. Sexual activities can be resumed once your bruising and swelling have subsided however you can discuss this with the surgeon before your operation.
Please do not hesitate to ask any further questions at anytime, we would be more than happy to help.